Monitoring eye pressure is a vital part of every comprehensive eye check, as it helps detect early signs of serious conditions like glaucoma, often before any symptoms arise.
But what exactly is eye pressure, what’s considered a normal range, and when should you be concerned?
What Is Eye Pressure?
Eye pressure, or intraocular pressure (IOP), refers to the pressure inside your eye. It plays an essential role in maintaining the shape of the eye and ensuring proper functioning of internal structures.
The intraocular pressure is primarily regulated by inflow and outflow of a fluid called aqueous humor. Aqueous humor is continuously produced by the eye and drained through a specialised drainage system. When this system is working well, a balance is maintained between fluid production and outflow.
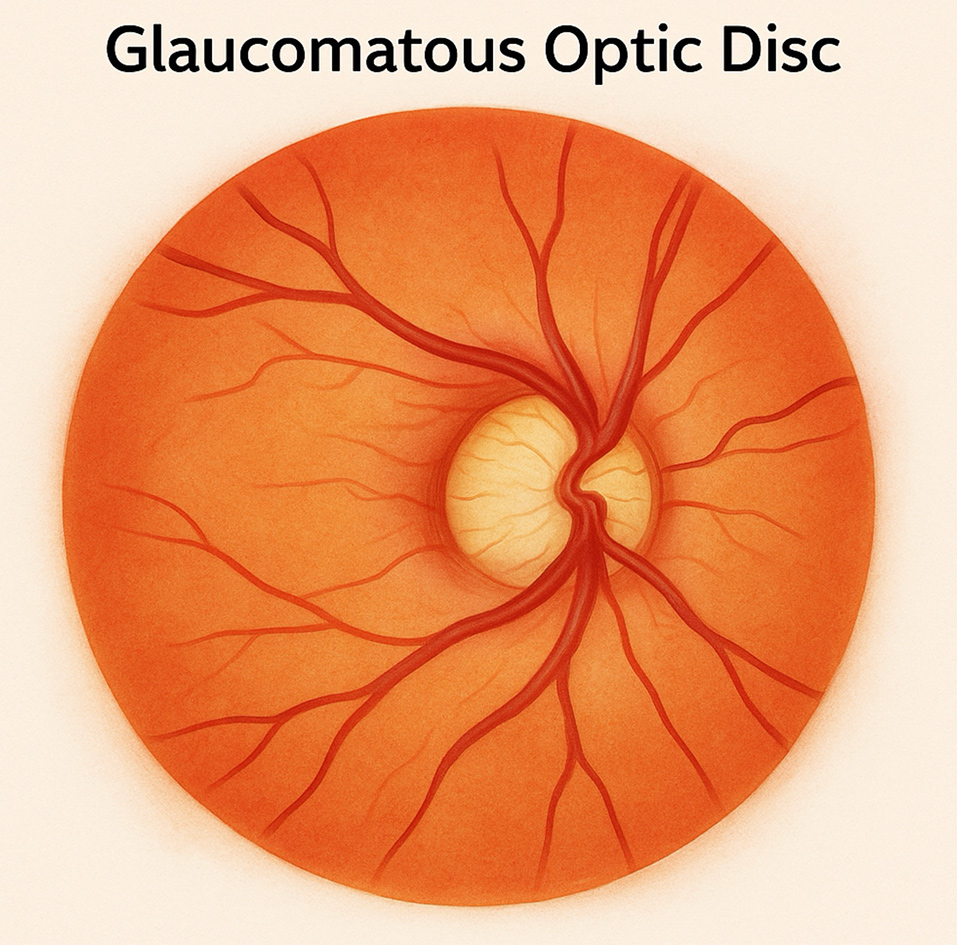
However, if the drainage channels become blocked or inefficient, then the intraocular pressure can become higher than normal. Elevated eye pressure is one of the main risk factors for glaucoma, a condition that can cause irreversible vision loss if not caught early.
At Vision Clinic Sydney, we measure eye pressure during every comprehensive eye examination using safe, quick, and accurate methods. Increases in pressure when monitored over time can provide crucial insights into your eye health.
What Is the Normal Eye Pressure Range?
A healthy intraocular pressure (IOP) typically falls between 10 and 21 mmHg. This measurement is expressed in millimetres of mercury (mmHg), similar to how blood pressure is measured.
However, the “normal” range isn’t one-size-fits-all. Some people naturally have slightly higher or lower pressure, which may still be safe depending on their optic nerve health and other individual factors.
Normal Eye Pressure by Age
Children and Teenagers: Typically between 10–20 mmHg
Adults Under 40: Generally remains stable, around 12–21 mmHg
Adults Aged 40 and Over: Still considered normal between 10–21 mmHg, but risk for glaucoma increases with age, especially if pressures trend toward the higher end of this spectrum.
It’s important to note that “normal” pressure varies between individuals. Some people may develop glaucoma even with IOPs in the normal range, this is called normal-tension glaucoma, while others with higher pressures may not experience any damage. That’s why regular eye pressure monitoring and a complete optic nerve assessment are key to preserving your long-term vision.

What Is Considered Dangerously High Eye Pressure?
Any reading above 21 mmHg is considered elevated. Readings above 30 mmHg are typically regarded as dangerously high, especially if persistent.
Without intervention, high pressure can damage the optic nerve, leading to glaucoma which is a major cause of irreversible blindness.
Symptoms of High Eye Pressure
Many people with high eye pressure don’t notice any symptoms, especially in the early stages. That’s what makes regular eye checks so important.
When symptoms do appear, they may include:
- Blurry or fluctuating vision
- Eye pain or pressure sensation
- Headaches
- Halos around lights
- Nausea or vomiting (in acute cases)
Acute angle-closure, a rare but serious condition, can cause a sudden spike in pressure with severe symptoms—this requires emergency care.
Low Eye Pressure Symptoms
On the other end of the spectrum, low eye pressure (ocular hypotony) can also affect vision.
Symptoms may include:
- Distorted or blurry vision
- Eye pain or discomfort
- Flattening of the eyeball or vision instability
Low pressure can result from trauma, inflammation, or complications after surgery. It can compromise the structure of the eye and lead to permanent vision issues if not managed appropriately.
How to Reduce High Eye Pressure
If you’ve been told you have elevated intraocular pressure (IOP), early intervention is key to protecting your vision. The good news is that high eye pressure can often be managed effectively through the following strategies:
1. Prescription Eye Drops
These are the most common and effective initial treatments. They work by either decreasing the production of aqueous humour (the fluid in your eye) or improving its drainage.
2. Selective Laser Trabeculoplasty (SLT)
A minimally invasive non thermal (cold) laser treatment to lower eye pressure.
3. Healthy Lifestyle Changes
Several everyday habits can help regulate eye pressure:
- Aerobic exercise (like walking or swimming) can support healthy IOP levels.
- A balanced diet rich in leafy greens and antioxidants supports overall eye health.
- Stay hydrated but avoid excessive fluid intake in short periods, which may temporarily raise IOP.
- Stop smoking and manage blood pressure or diabetes, both of which can affect eye health.
4. Regular Eye Exams
Monitoring your IOP over time is essential. At Vision Clinic Sydney, we use advanced tools to track your eye pressure and detect changes early.
5. Avoid High-Risk Behaviours
Minimise extended head-down positions (e.g., certain yoga poses), which can raise IOP and be cautious with steroid medications (including eye drops), as they can increase pressure in some individuals.
If your IOP remains elevated despite these approaches, Dr. Kumar may explore further tailored interventions to prevent optic nerve damage. Early action is the best way to maintain lifelong vision health.
Why Monitoring Eye Pressure Matters
One of the leading causes of preventable blindness, glaucoma, is often linked to untreated high eye pressure. Because there are no early warning signs in most cases, annual eye exams are the only way to catch changes before permanent damage occurs.
Vision Clinic Sydney uses advanced diagnostic tools and offers tailored treatment plans to manage pressure before complications arise.
How To Book an Assessment
To request an appointment or if you have an enquiry, please contact us via the following ways:
Call or message us: +612 9222 9188
Email us: reception@visionclinicsydney.com.au
Book online via our website
FAQs
What does high eye pressure feel like?
In most people, high eye pressure doesn’t feel like anything at all. However, in rare acute cases, it can cause eye pain, headaches, blurry vision, or nausea. These are signs of a potential emergency.
Can eye pressure fluctuate during the day?
Yes, eye pressure naturally varies throughout the day. This is why it may be measured at different times or over multiple visits to get a more accurate assessment.
Is high eye pressure always a sign of glaucoma?
Not necessarily. Some people have high IOP without glaucoma (ocular hypertension), while others develop glaucoma even with normal pressure. Regular monitoring is key to understanding your individual risk.
Can lifestyle changes lower my eye pressure?
In some cases, yes. Maintaining a healthy weight, reducing caffeine intake, quitting smoking, managing stress, and regular physical activity may help lower IOP. Always consult with your eye doctor before making changes.
How often should I check my eye pressure?
If you’re over 40 or have risk factors for glaucoma, an annual comprehensive eye exam at Vision Clinic Sydney is recommended. More frequent checks may be advised based on your results.
General Information Disclaimer: The content provided here is for informational purposes only and is not intended as medical advice, diagnosis, or treatment. Always seek the advice of your health professional with any questions you may have regarding a medical condition. The information on this site is general in nature and may not reflect current medical developments or research. Your reliance on any information provided by this site is solely at your own risk.

























